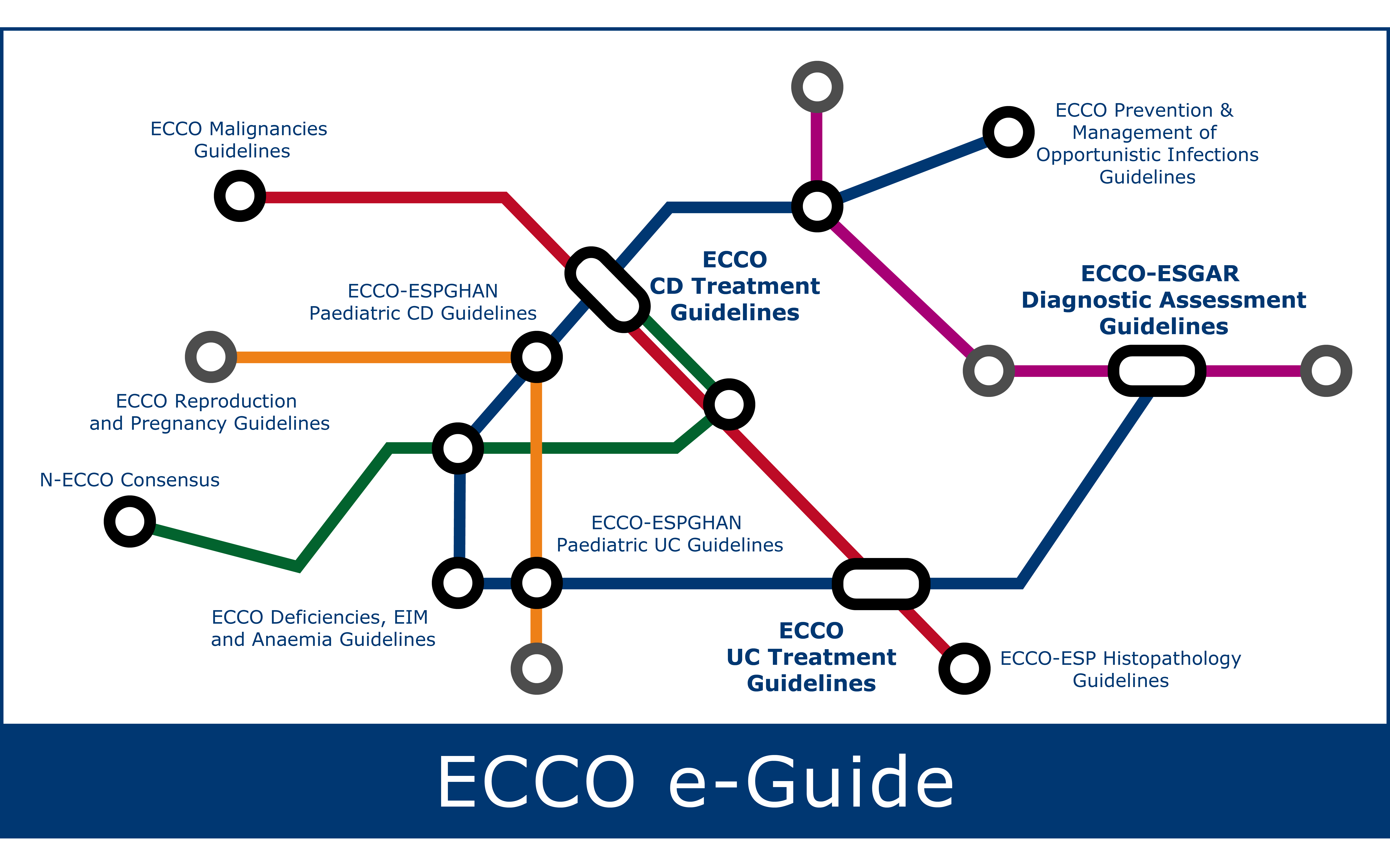
The information below is based on the summary of product characteristics approved by regulatory authorities and ECCO Guidelines.
Additional related ECCO e-Learning resources can be found under IBD Curriculum Topic 6.1-6.11
Introduction and Mechanism of Action
Bowel disease (inflammatory) suppressant: Mechanism of action is uncertain. Mucosal production of arachidonic acid metabolites, both through the cyclooxygenase and lipoxygenase pathways, is increased in patients with inflammatory bowel disease. Mesalamine appears to diminish inflammation by inhibiting cyclooxygenase and lipoxygenase, thereby decreasing the production of prostaglandins, and leukotrienes and hydroxyeicosatetraenoic acids (HETEs), respectively.
It is also believed that mesalamine acts as a scavenger of oxygen-derived free radicals which are produced in greater numbers in patients with inflammatory bowel disease.
5-ASA compounds can be delivered both orally and rectally with several topical formulations (suppositories, foams, enemas). Various modes of release in the gut exist, namely the pH-dependent and the time-dependent.
Therapeutic indications
Treatment of mild-to-moderate acute exacerbations of ulcerative colitis and for maintenance of remission in ulcerative colitis.
Recent evidence have suggested no clear beneficial effect of 5-ASA in the treatment of Crohn's disease.
Dosing, administration, and monitoring
Oral 5-ASA should be administered at a dose of ≥2 g/day to induce remission in patients with mildly-to-moderately active UC. In active distal colitis of at least rectosigmoid extent, topical [rectal] 5-ASA at a dose of ≥1 g/d should also be added for a combined effect.
Similarly, oral 5-ASA at a dose ≥2 g/day is suggested for maintenance of remission in UC patients, with the use of topical [rectal] 5-ASA in case of distal UC.
Monitoring
Blood tests (differential blood count; liver function parameters such as ALT or AST; serum creatinine) and urinary status (dip sticks) should be determined prior to and during treatment, at the discretion of the treating physician. As a guideline, follow-up tests are recommended 14 days after commencement of treatment, then a further two to three tests at intervals of 4 weeks.
If the findings are normal, follow-up tests should be carried out every 3-6 months. If additional symptoms occur, these tests should be performed immediately.
Adverse effects
Mesalazine in general is contraindicated in cases of:
- Hypersensitivity to the active substance, salicylates or to any of the excipients listed in each specific mesalazine product.
- Severe impairment of hepatic or renal function.
Sulfasalazine is contraindicated in:
- Infants under the age of 2 years.
- Patients with a known hypersensitivity to sulfasalazine, its metabolites or any of the excipients as well as sufonamides or salicylates.
- Patients with porphyria.
Special warnings and precautions for use
Caution is recommended in patients with impaired hepatic function. Mesalazine should not be used in patients with impaired renal function. Mesalazine-induced renal toxicity should be considered if renal function deteriorates during treatment.
Patients with pulmonary disease, in particular asthma, should be very carefully monitored during a course of treatment with mesalazine tablets.
Patients with a history of adverse drug reactions to preparations containing sulphasalazine should be kept under close medical surveillance on commencement of a course of treatment with mesalazine tablets. Should mesalazine tablets cause acute intolerance reactions such as abdominal cramps, acute abdominal pain, fever, severe headache and rash, therapy should be discontinued immediately.
Mesalazine Undesirable effects
|
Organ Class System |
Frequency According to MedDRA convention |
|
|
|
Rare |
Very rare |
|
Blood and lymphatic system disorders |
|
Altered blood counts (aplastic anaemia, agranulocytosis, pancytopenia, neutropenia, leukopenia, thrombocytopenia) |
|
Nervous system disorders |
Headache, dizziness |
peripheral neuropathy |
|
Cardiac disorders |
Myocarditis, Pericarditis |
|
|
Respiratory, thoracic and mediastinal disorders |
|
Allergic and fibrotic lung reactions (including dyspnoea, cough, bronchospasm, alveolitis, pulmonary eosinophilia, lung infiltration, pneumonitis) |
|
Gastrointestinal disorders |
Abdominal pain, diarrhoea, flatulence, nausea, vomiting |
Acute pancreatitis |
|
Renal and urinary disorders |
|
Impairment of renal function including acute and chronic interstitial nephritis and renal insufficiency |
|
Skin and subcutaneous tissue disorders |
Photosensitivity |
Alopecia |
|
Musculoskeletal and connective tissue disorders |
|
Myalgia, arthralgia |
|
Immune system disorders |
|
Hypersensitivity reactions such as allergic exanthema, drug fever, lupus erythematosus syndrome, pancolitis |
|
Hepatobiliary disorders |
|
Changes in liver function parameters (increase in transaminases and cholestasis parameters), hepatitis, cholestatic hepatitis |
|
Reproductive system disorders |
|
Oligospermia (reversible) |
Photosensitivity
More severe reactions are reported in patients with pre-existing skin conditions such as atopic dermatitis and atopic eczema.
Overdose
There are rare data on overdosage (e.g., intended suicide with high oral doses of mesalazine), which do not indicate renal or hepatic toxicity. There is no specific antidote and treatment is symptomatic and supportive.
Salazopyrin undesirable effects
Overall, about 75% of ADRs occur within 3 months of starting therapy, and over 90% by 6 months. Some undesirable effects are dose-dependent and symptoms can often be alleviated by reduction of the dose.
General
Sulfasalazine is split by intestinal bacteria to sulfapyridine and 5-amino salicylate so ADRs to either sulfonamide or salicylate are possible. Patients with slow acetylator status are more likely to experience ADRs related to sulfapyridine. The most commonly encountered ADRs are nausea, headache, rash, loss of appetite and raised temperature.
Specific
The adverse reactions observed during clinical studies conducted with Sulfasalazine have been provided in a single list below by class and frequency (very common (≥1/10); common (≥1/100 to< 1/10); uncommon (≥1/1000 to < 1/100). Where an adverse reaction was seen at different frequencies in clinical studies, it was assigned to the highest frequency reported.
Additional reactions reported from post-marketing experience are included as frequency Not known (cannot be estimated from the available data) in the list below.
|
Body System |
Adverse drug reactions |
|
Infections and infestations |
|
|
Not known |
Pseudomembranous colitis |
|
Blood and Lymphatic System Disorders |
|
|
Common |
Leukopenia |
|
Uncommon |
Thrombocytopenia |
|
Not known |
Agranulocytosis, aplastic anaemia, haemolytic anaemia, Heinz body anaemia, hypoprothrombinaemia, lymphadenopathy, macrocytosis, megaloblastic anaemia, methaemoglobinaemina, neutropenia, pancytopenia |
|
Immune System Disorders |
|
|
Not known |
Anaphylaxis, polyarteritis nodosa, serum sickness |
|
Metabolism and Nutrition Disorders |
|
|
Not known |
Loss of appetite |
|
Psychiatric Disorders |
|
|
Common |
Insomnia |
|
Uncommon |
Depression |
|
Not known |
Hallucinations |
|
Nervous System Disorders |
|
|
Common |
Dizziness, headache, taste disorders |
|
Uncommon |
Convulsions |
|
Not known |
Aseptic meningitis, ataxia, encephalopathy, peripheral neuropathy, smell disorders |
|
Ear and Labyrinth Disorders |
|
|
Common |
Tinnitus |
|
Uncommon |
Vertigo |
|
Eye Disorders |
|
|
Common |
Conjunctival and scleral injection |
|
Cardiac Disorders |
|
|
Not known |
Allergic myocarditis, cyanosis, pericarditis |
|
Vascular Disorders |
|
|
Uncommon |
Vasculitis |
|
Respiratory, Thoracic and Mediastinal Disorders |
|
|
Common |
Cough |
|
Uncommon |
Dyspnoea |
|
Not known |
Fibrosing alveolitis, eosinophilic infiltration, interstitial lung disease |
|
Gastrointestinal Disorders |
|
|
Very Common |
Gastric distress, nausea |
|
Common |
Abdominal pain, diarrhoea, vomiting, stomatitis |
|
Not known |
Aggravation of ulcerative colitis, pancreatitis, parotitis |
|
Hepato-biliary Disorders |
|
|
Not known |
Hepatic failure, fulminant hepatitis, hepatitis |
|
Skin and Subcutaneous Tissue Disorders |
|
|
Common |
Pruritus |
|
Uncommon |
Alopecia, urticaria |
|
Not known |
Epidermal necrolysis (Lyell's syndrome), Stevens-Johnson syndrome, drug rash with eosinophilia and systemic symptoms (DRESS), toxic pustuloderma, erythema, exanthema, exfoliative dermatitis, periorbital oedema, lichen planus, photosensitivity |
|
Musculoskeletal and Connective Tissue Disorders |
|
|
Common |
Arthralgia |
|
Not known |
Systemic lupus erythematosus |
|
Renal and Urinary Disorders |
|
|
Common |
Proteinuria |
|
Not known |
Nephrotic syndrome, interstitial nephritis, crystalluria, haematuria |
|
Reproductive System and Breast Disorders |
|
|
Not known |
Reversible oligospermia |
|
General Disorders and Administration Site Conditions |
|
|
Common |
Fever |
|
Uncommon |
Facial oedema |
|
Not known |
Yellow discoloration of skin and body fluids |
|
Investigations |
|
|
Uncommon |
Elevation of liver enzymes |
|
Not known |
Induction of autoantibodies |
Special situations (e.g. pregnancy)
Pregnancy and Breastfeeding / Lactation
As per the latest ECCO Guidelines on this matter (https://doi.org/10.1093/ecco-jcc/jjac115), 5-ASA is regarded as low risk during pregnancy and lactation. Although higher rates of premature birth, stillbirth, and LBW were observed in some studies, it seems plausible that these results were due to the confounding factor of active disease. Teratogenic effects have not been demonstrated.
To prevent toxicity of sulphasalazine treatment preventing folate absorption, supplementation with folate 2 mg/day is recommended. If using an aminosalicylate with dibutyl coating, switching to a different 5-ASA formulation should be considered for the pregnant IBD patient due to the possibility of urogenital malformations in the offspring.