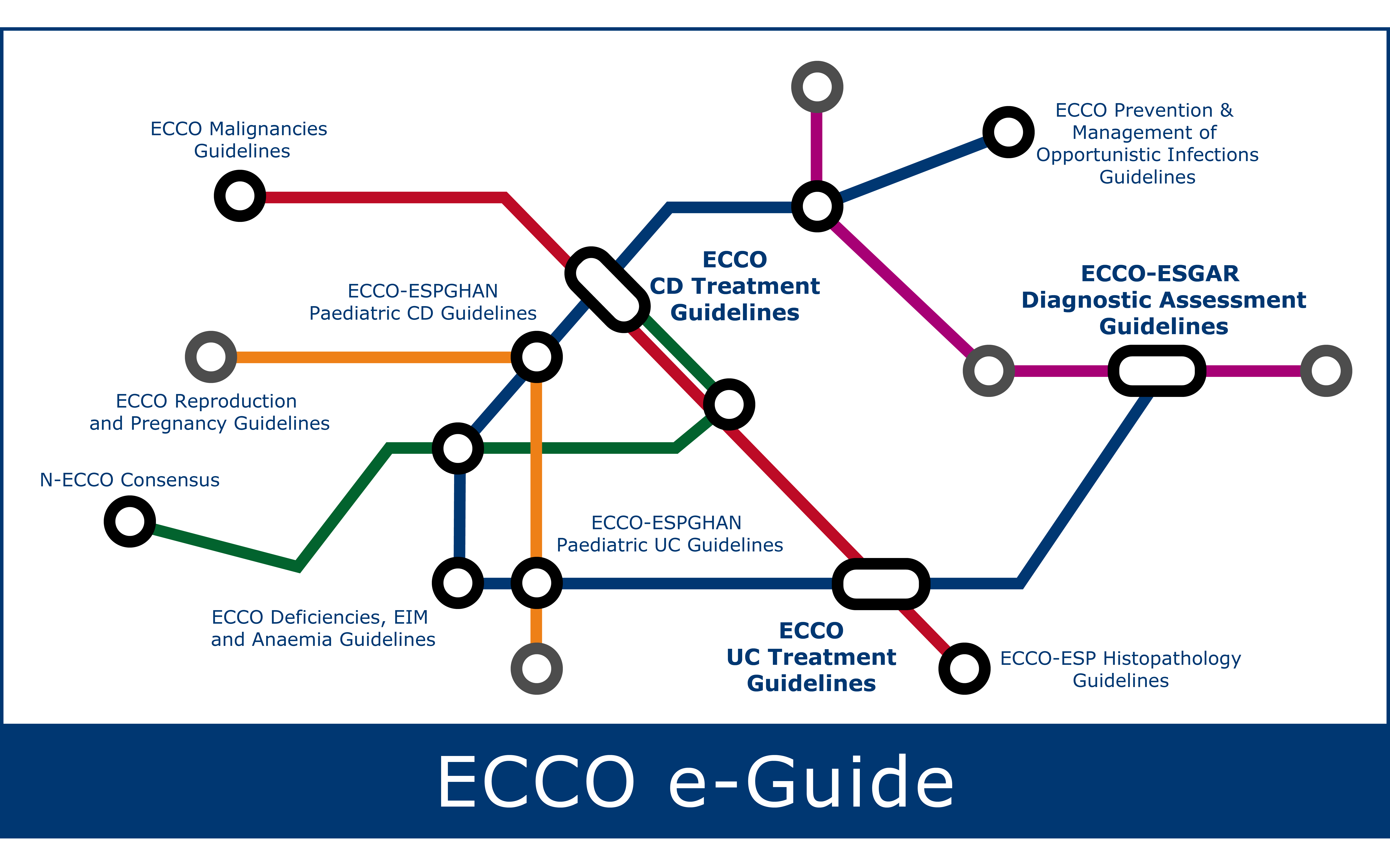
Additional related ECCO e-Learning resources can be found under:
IBD Curriculum Topic 6.1-6.11
IBD Curriculum Topic 7.4
IBD Curriculum Topic 9.4
In general, antibiotics are only appropriate for septic complications and specific indications such as bacterial overgrowth. Antibiotics may be considered in specific cases of post-operative Crohn's disease or fistulising perianal Crohn's disease. They are not recommended as a monotherapy to induce or maintain remission in Crohn's disease.
Active disease
- Metronidazole, in small trials has been associated with possible improvement in symptoms in colonic Crohn's disease, but this benefit has not been demonstrated larger adequately powered studies, nor in small bowel disease. Prolonged courses of metronidazole are also associated with issues of poor tolerance. Peripheral neuropathy limits the long-term use of metronidazole and can persist in some patients.
- Ciprofloxacin has similar efficacy in active luminal disease as mesalazine, and mesalazine having similar efficacy to placebo. Therefore, neither are currently recommended for the treatment of active Crohn's disease. Tendon inflammation and damage can occur due to ciprofloxacin.
- Uncontrolled case series support use of metronidazole and/or ciprofloxacin in perianal disease, though they rarely induce complete healing. They are usually used as an adjunct to thiopurines and anti-TNF therapy in fistulising perianal Crohn’s disease.
- Rifaximin has been associated with possible benefit for active luminal Crohn's disease but this has not bee demonstrated in large, adequately powered studies.
- Anti-mycobacterial therapy is not recommended for the treatment or prevention of Crohn's disease..
- National formularies and local guidelines should be consulted to review appropriate drug dosing, adverse drug reactions and drug interactions.
Maintaining remission
Evidence for effectiveness of antibiotics, particularly anti-mycobacterial agents, is lacking.
Prevention of post-surgical recurrence
- Metronidazole 20mg/kg/d for 3 months reduces endoscopic & clinical recurrence at 12 months, but not at 24 months.
- Ornidazole 1g/d for 12 months reduces clinical recurrence, at 12 but not at 24 months.
- Poor tolerance of long-term therapy reduces the effectiveness for these therapies to reduce post-operative recurrence.
Prolonged antibiotic therapy
In septic complications and perianal disease, antibiotics can be prolonged up to the resolution of infection.
Dosing, administration and monitoring
Before treatment
No particular screening is required before administering antibiotics in Crohn's disease.
Dosing
- Symptomatic perianal fistula:
- Ciprofloxacin 1000 mg/day (in 2 divided doses)
- Metronidazole: 750-1500 mg/day (in 2-3 divided doses)
- For post-operative prophylaxis in CD:
- Metronidazole 20 mg/kg for 3 months
Follow-up
- Metronidazole:
- Warn about alcohol consumption while on metronidazole due to potential disulfiram-like reaction
- Monitor serum ciclosporin level if administered as concomitant therapy
- Monitor lithium levels when lithium is prescribed concomitantly
- Ciprofloxacin:
- Consider reduced renal tubular transport of methotrexate when co-administered
Red flag interactions
- Ciprofloxacin should be stopped in cases of Achillles tendinopathy
- Metronidazole should be stopped in case of peripheral neuropathy
Adverse effects
Metronidazole can cause gastrointestinal symptoms such as nausea, vomiting, and stomatitis. In case of prolonged use, reversible leucopenia or peripheral neuropathy may occur.
Ciprofloxacin may cause tendinitis, especially at Achilles tendon, photosensitivity, central or peripheral neuropathy, QT-interval prolongation, and should be carefully used in case of kidney or hepatic failure, or with concomitant drugs metabolized by CYP1A2.
Special situations
Pregnancy
Both ciprofloxacin and metronidazole should be avoided especially in the first trimester, unless absolutely necessary.
Breastfeeding
Both ciprofloxacin and metronidazole should be avoided.
Surgery
No concerns
Paediatrics
No contraindications
Elderly
No contraindications